The now-deleted updates were notable because so far the CDC has stopped short of saying that the virus is airborne.
Over the weekend, the CDC page "How COVID-19 Spreads" included among the most common modes of transmission "respiratory droplets or small particles, such as those in aerosols, produced when an infected person coughs, sneezes, sings, talks, or breathes."
The posted and withdrawn transmission guidelines are just the latest in public reversals and controversy at the CDC.
On Friday, the agency reversed its new guidance on testing, published in August, that suggested people who have possibly been exposed to the coronavirus don't necessarily need to get tested for infection.
WHAT CDC HAS NOT DONE, among many things, is tell Americans why so many doctors and staff have contracted this virus even while taking the utmost precautions, with some even wearing full HAZMAT suits.
They have also, in the professional opinion of MANY, caused a false sense of security by pressing the wearing of masks as the MAIN way to prevent spreading the disease.
If that were true, healthcare workers would be some of the SAFEST people on earth.
As the stats below will show, that is NOT the case.
-- Health-care workers make up 1 in 7 covid-19 cases recorded globally, WHO says.
According to Italy’s national health institute, 4,824 health care workers have been infected, twice as many as in China.
If that were true, healthcare workers would be some of the SAFEST people on earth.
As the stats below will show, that is NOT the case.
Wearing any or all of the available protection devices shown above has NOT stopped contamination in hospital workers, physicians' private practices, or in first responders.
Even with the most drastic measures to decontaminate, health workers are still getting infected.
-- Health-care workers make up 1 in 7 covid-19 cases recorded globally, WHO says.
-- Skyrocketing coronavirus deaths and infections among doctors and nurses reveal stories of bravery, betrayal and a total lack of preparedness.
According to Italy’s national health institute, 4,824 health care workers have been infected, twice as many as in China.
In Spain, the health ministry announced this week that out of 40,000 confirmed cases of coronavirus in the country, 5,400 — nearly 14% — are medical professionals. In France, five doctors have died from the virus as well.
-- There were 62,344 cases of COVID-19 among healthcare personnel in the U.S., and 291 had died, data from the CDC in May showed. The number of healthcare worker coronavirus infections has risen sharply.
-- “Globally, around 14 percent of covid-19 cases reported to WHO are among health workers, and in some countries it’s as much as 35 percent,” WHO director general Tedros Adhanom Ghebreyesus said at a news conference in Geneva.
The figures are disproportionate: Data collected by the WHO suggests that health workers represent less than 3 percent of the population in the majority of countries and less than 2 percent in almost all low- and middle-income countries.
But the WHO’s data, released to mark World Patient Safety Day on Thursday, fits with other estimates. In April, the U.S. Centers for Disease Control and Prevention found that health-care workers accounted for 11 percent to 16 percent of covid-19 cases during the first surge of infections in the United States.
Add the 14% of cases in healthcare workers about that time and we can see that about 28% of the cases were under 50 and seemed to be less susceptible than the other two groups.
Economic variants do NOT explain this.
As of October 1, 2020, 104,845,807 PCR test samples have been submitted in the USA, from all 50 states and 6 territories, 7,244,495 were confirmed positive, OR PROBABLE.
THAT'S TESTING ONLY ABOUT 1/3rd OF THE U.S. POPULATION, IF EACH TEST REPRESENTS ONE PATIENT.
As of October 1, 2020, 104,845,807 PCR test samples have been submitted in the USA, from all 50 states and 6 territories, 7,244,495 were confirmed positive, OR PROBABLE.
THAT'S TESTING ONLY ABOUT 1/3rd OF THE U.S. POPULATION, IF EACH TEST REPRESENTS ONE PATIENT.
NOT SUFFICIENT AND NOT ACCEPTABLE.
I find NO data on how many of these tests were REPEAT tests on the same patient.
Because of my age, health conditions and frequency of doctor/hospital visits, I was once being tested weekly, until I had the antibody test that showed I had already had CV-19, probably in January or February.
I was 100% symptom free all those months, not even a slight temperature.
No wonder PCRs came back negative. I had 'recovered'.
How many others will never know they're recovered because CDC frowns on antibody testing?
WHAT IS A PCR TEST AND HOW RELIABLE IS IT?
Doctors use this test to diagnose people who are currently sick with COVID-19.
This test uses a sample of mucus typically taken by swab from a person's nose or throat.
How many others will never know they're recovered because CDC frowns on antibody testing?
WHAT IS A PCR TEST AND HOW RELIABLE IS IT?
Doctors use this test to diagnose people who are currently sick with COVID-19.
This test uses a sample of mucus typically taken by swab from a person's nose or throat.
The test won't identify someone who has recently been infected. And swabs can sometimes fail to pick up signs of active infection.
New research from Johns Hopkins University (MD, USA) has found that the chance of these tests giving a false negative – stating no infection when the individual actually is infected – is greater than 1 in 5, at times being far higher.
The probability of a false negative COVID-19 test decreased from 100% on Day 1 of the infection to 67% on Day 4. This further decreased to 20% on Day 8, 3 days after a patient would first start to experience COVID-19 symptoms.
Day 8 appeared to be the optimal time for testing, as after this the probability of a false negative once again began to increase. A 21% probability on Day 9 increased to 66% if testing occurred on Day 21 of infection.
A similar study, published earlier this month in the BMJ, also highlighted the inaccuracies of PCR-based testing.
PCR tests are the tests done in international airports and emergency rooms, so we need to question if too many are coming into the U.S. or traveling inside the U.S. with a FALSE NEGATIVE test, or if healthcare workers and those who are showing symptoms of the virus but test negative are also going about their lives WITH the virus.
Antibody tests are able to determine whether an individual has already had the virus (though possibly symptom free) by detecting the presence of antibodies against SARS-CoV-2 in a blood sample.
Different tests do vary in accuracy and tests relying on blood samples drawn by healthcare professionals have been shown to be more accurate than those that use finger prick samples.
The results are alarming. Even when a mask is worn, some droplets can travel a considerable distance during periods of mild coughing,’ the authors wrote.
The tests were based on a standard surgical mask exhibiting initial efficiency of about 91 per cent when preventing droplets from escaping.
The study, published in Physics of Fluids, found face masks can reduce transmission of airborne droplets – but not eliminate them completely.
Without a mask these droplets travel twice as far.
However, repeated coughing, a symptom of coronavirus, reduces the efficiency of a mask and so more droplets are let through.
Previous work by the same team showed droplets of saliva can travel 18 feet in five seconds when an unmasked person coughs.
The researchers also urged manufacturers and regulatory authorities to consider new criteria for assessing mask performance that account for flow physics and cough dynamics.
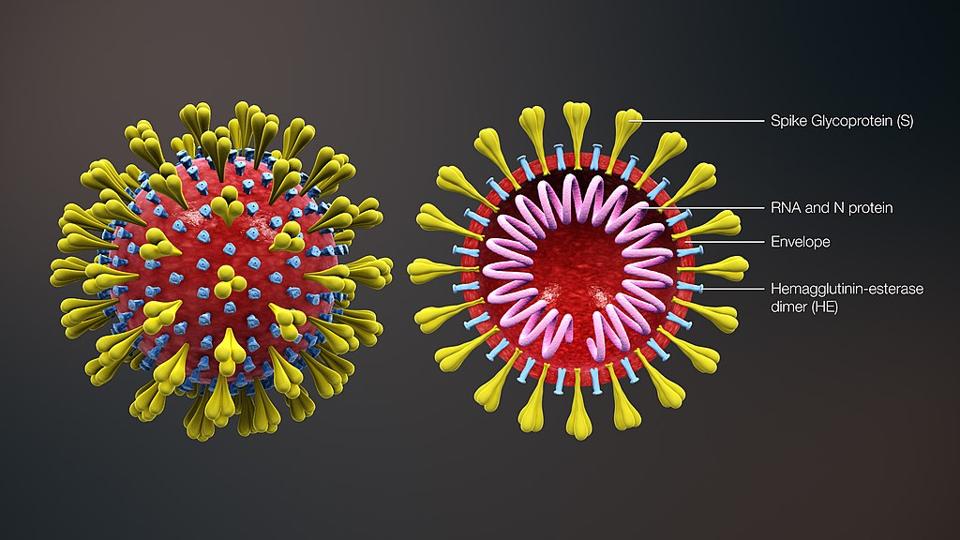
THIS DOES NOT ADDRESS THE FACT THAT COVID-19 IS ONE OF THE TINIEST VIRUSES KNOWN.
N95 masks, the masks most needed by healthcare workers, actually have that name because they are considered to be 95% efficient at stopping particles in their least efficient particle size range — in this case those around 0.3 microns.
(As you'll see below, such is NOT the case.)
The science of mask functionality gets really small, really fast. The unit of measurement here is microns — 1/1000th of a millimeter.
The COVID-19 particle is indeed small, only around 0.1 microns in size, but it is always bonded to something larger, like aerosol droplets.
Breathing and talking generate particles around 1 micron in size.
“When the electrostatic charges of the N95 masks are dissipated during usage or storage, the capability of stopping virus-sized particles diminishes.
Masks do NOTHING to stop particles from entering the body at the EYES.
The clear tissue that covers the white of the eye and lines the inside of the eyelid, known as the conjunctiva, “can be infected by other viruses, such as adenoviruses associated with the common cold and the herpes simplex virus.
"There’s the same chance of infection with SARS-CoV-2," says Elia Duh, MD, a researcher and professor of ophthalmology at the Johns Hopkins School of Medicine in Baltimore.. “If there are droplets that an infected individual is producing by coughing or sneezing or even speaking, then the front of the eyes are directly exposed, just like the nasal passages are exposed. In addition, people rub and touch their eyes a lot. So there’s certainly already the vulnerability.”
The novel coronavirus can be transmitted through the eyes because of a protein known as the “gateway” into cells inside the body, according to a Johns Hopkins study.
Doctors first claimed the virus could be spread through the eyes in January, when the epicenter was still in Wuhan, China.
Dr. Wang Guangfa said at the time that he believed he had been infected because he had not been wearing protective goggles.
The tests were based on a standard surgical mask exhibiting initial efficiency of about 91 per cent when preventing droplets from escaping.
The study, published in Physics of Fluids, found face masks can reduce transmission of airborne droplets – but not eliminate them completely.
Without a mask these droplets travel twice as far.
However, repeated coughing, a symptom of coronavirus, reduces the efficiency of a mask and so more droplets are let through.
Previous work by the same team showed droplets of saliva can travel 18 feet in five seconds when an unmasked person coughs.
The researchers also urged manufacturers and regulatory authorities to consider new criteria for assessing mask performance that account for flow physics and cough dynamics.
THIS DOES NOT ADDRESS THE FACT THAT COVID-19 IS ONE OF THE TINIEST VIRUSES KNOWN.
N95 masks, the masks most needed by healthcare workers, actually have that name because they are considered to be 95% efficient at stopping particles in their least efficient particle size range — in this case those around 0.3 microns.
(As you'll see below, such is NOT the case.)
The science of mask functionality gets really small, really fast. The unit of measurement here is microns — 1/1000th of a millimeter.
The COVID-19 particle is indeed small, only around 0.1 microns in size, but it is always bonded to something larger, like aerosol droplets.
Breathing and talking generate particles around 1 micron in size.
“When the electrostatic charges of the N95 masks are dissipated during usage or storage, the capability of stopping virus-sized particles diminishes.
This is the main reason of not recommending the reuse of N95 masks.”
WE KNEW IN 2008 THAT THE N95 AND SURGICAL MASKS DID NOT FILTER CORONAVIRUS OR FLU VIRUSES AS WELL AS PREVIOUSLY THOUGHT.
Respiratory Performance Offered by N95 Respirators and Surgical Masks: Human Subject Evaluation
WE KNEW IN 2008 THAT THE N95 AND SURGICAL MASKS DID NOT FILTER CORONAVIRUS OR FLU VIRUSES AS WELL AS PREVIOUSLY THOUGHT.
Respiratory Performance Offered by N95 Respirators and Surgical Masks: Human Subject Evaluation
"Most of the tested N95 respirators and surgical masks in this study were observed to perform at their worst against particles approximately between 0.04 and 0.2 μm, which includes the sizes of coronavirus and influenza virus.
The tested N95 respirators provided about 8–12 times better protection than the surgical masks. However, ∼29% of the tested N95 respirators had PFs <10, indicating that the newly assigned OSHA PF (Protection Factor) of 10 may overestimate the actual protection offered by N95 respirators against bacteria and viruses.
When testing at an inhalation flow rate of 85 l min−1, the penetration of MS2 virions (0.01–0.08 μm) through the N95 respirator filter exceeded 5%.
When testing at an inhalation flow rate of 85 l min−1, the penetration of MS2 virions (0.01–0.08 μm) through the N95 respirator filter exceeded 5%.
For surgical masks, the penetration was much higher and varied from 20.5 to 84.5%.
(Surgical masks allowed much more of the viruses in.)
(Surgical masks allowed much more of the viruses in.)
In these studies, the respirators were sealed on a manikin face to account only for particles penetrating through the respirator filter material.
However, airborne particles can also enter the respirator cavity through face-seal leaks and be subsequently inhaled into human respiratory systems.
Surgical masks filtration ability (protection of the wearer) was nine times lower than that provided by N95 respirators.
The data obtained in the present study by count-based measurement show that particles approximately between 0.08 and 0.2 μm in aerodynamic diameter are more likely to penetrate into most of the tested N95 respirators.
Surgical masks filtration ability (protection of the wearer) was nine times lower than that provided by N95 respirators.
The data obtained in the present study by count-based measurement show that particles approximately between 0.08 and 0.2 μm in aerodynamic diameter are more likely to penetrate into most of the tested N95 respirators.
The respective size was 0.04–0.2 μm for surgical masks. Strikingly, the physical size of SARS-causing coronavirus is approximately 0.08–0.14 μm, and the physical size of influenza virus is 0.08–0.12 μm, i.e. the size ranges of these viruses fall into the most penetrating particle size range.
After accounting for the individual differences, the average PF offered by N95 filtering facepiece respirators against particles in the tested size range was about 8–12 times greater than that provided by surgical masks. This result is similar to that obtained by Lawrence et al. (2006) who found, using a nonsize-selective device (TSI PortaCount Plus), that the protection provided by N95 filtering facepiece respirators is about seven times greater than that of surgical masks."
After accounting for the individual differences, the average PF offered by N95 filtering facepiece respirators against particles in the tested size range was about 8–12 times greater than that provided by surgical masks. This result is similar to that obtained by Lawrence et al. (2006) who found, using a nonsize-selective device (TSI PortaCount Plus), that the protection provided by N95 filtering facepiece respirators is about seven times greater than that of surgical masks."
Work by Morawska (2006) demonstrated that bio-aerosol droplets can quickly dry in air to sub-micrometer and even ultra-fine sizes and remain airborne for prolonged periods, thus representing a higher risk for infection.
It's these particles that all masks have trouble filtering out.
REUSING THE MASK YOU WORE YESTERDAY IS VERY UNWISE UNLESS YOU WASHED IT THOROUGHLY, IF IT CAN BE LAUNDERED.
It's these particles that all masks have trouble filtering out.
REUSING THE MASK YOU WORE YESTERDAY IS VERY UNWISE UNLESS YOU WASHED IT THOROUGHLY, IF IT CAN BE LAUNDERED.
Taking off masks for a few minutes and then putting them back on must be done properly and carefully to keep from contaminating the inside surface and is not advised.
Masks do NOTHING to stop particles from entering the body at the EYES.
The clear tissue that covers the white of the eye and lines the inside of the eyelid, known as the conjunctiva, “can be infected by other viruses, such as adenoviruses associated with the common cold and the herpes simplex virus.
"There’s the same chance of infection with SARS-CoV-2," says Elia Duh, MD, a researcher and professor of ophthalmology at the Johns Hopkins School of Medicine in Baltimore.. “If there are droplets that an infected individual is producing by coughing or sneezing or even speaking, then the front of the eyes are directly exposed, just like the nasal passages are exposed. In addition, people rub and touch their eyes a lot. So there’s certainly already the vulnerability.”
The novel coronavirus can be transmitted through the eyes because of a protein known as the “gateway” into cells inside the body, according to a Johns Hopkins study.
Doctors first claimed the virus could be spread through the eyes in January, when the epicenter was still in Wuhan, China.
Dr. Wang Guangfa said at the time that he believed he had been infected because he had not been wearing protective goggles.
Virologist Joseph Fair, PhD, an NBC News contributor, raised that concern when he became critically ill with COVID-19, the disease caused by the coronavirus. From a hospital bed in his hometown of New Orleans, he told the network that he had flown on a crowded plane where flight attendants weren’t wearing masks. He wore a mask and gloves, but no eye protection.
“My best guess,” he told the interviewer, “was that it came through the eye route.”
Asked if people should start wearing eye protection, Fair replied, “In my opinion, yes.”“My best guess,” he told the interviewer, “was that it came through the eye route.”
HANDS, gloved or not, that come in contact with the virus in any way and then touch eyes, the nostrils/inside of noses or the lips also spread the virus.
When you remove gloves, just as when you remove masks, be aware that the virus can exist on their outer surfaces and that you need to wash up after their removal.
Proper and frequent hand-washing cannot be stressed enough.
Be sure to clean under nails.
THE IMPORTANCE OF CLEANING AND DISINFECTING SURFACES
The most important rule: Clean first.
Clean kitchens at least twice a day.
The CDC suggests mixing 4 teaspoons of bleach per quart of water. Let it sit for one minute on the surface until you dry it off.
Be aware of the time a disinfectant needs to stay on a surface while air-drying. Sansoni notes that you should “read the product label on all disinfectants and wipes, because they have instructions on letting the surface stay wet or air dry for a certain amount of time, which varies by product.”
There’s always the chance a nonporous (glass and metal) container could have been handled by someone with the virus — including a stocking person at the store. You can use the same disinfectant wipes or solution to clean cans, bottles and jars.
Wash your hands thoroughly.
Once you’ve finished cleaning surfaces, wash your hands thoroughly with soap and water for at least 20 seconds, following these CDC recommendations.
Dry your clean hands on a clean towel.
"The virus that has devastated the world this year, SARS-CoV-2, is not a living organism. Viruses are not alive.
We must consider that there are "virus super-spreaders" among our population.
These are infected individuals who may not even know they have CV-19.
What is a superspreader?
The word is a generic term for an unusually contagious individual who’s been infected with disease. In the context of the coronavirus, scientists haven’t narrowed down how many infections someone needs to cause to qualify as a superspreader, but generally speaking it far exceeds the two to three individuals researchers initially estimated the average infected patient could infect.
What’s the impact of superspreaders for covid-19?
--Disinfect the kitchen and rinse produce thoroughly.
Covid-19 Coronavirus Can Survive On Frozen Meat And Fish For Up To 3 Weeks, Study Finds
Covid-19 Coronavirus Can Survive On Frozen Meat And Fish For Up To 3 Weeks, Study Finds
The virus, officially dubbed SARS-CoV-2, is thought to be more stable on plastic and stainless steel than on copper and cardboard.
A recent study found that the COVID-19 coronavirus can survive up to four hours on copper, up to 24 hours on cardboard, and up to two to three days on plastic and stainless steel.
A recent study found that the COVID-19 coronavirus can survive up to four hours on copper, up to 24 hours on cardboard, and up to two to three days on plastic and stainless steel.
The virus has a lipid (fatty) outer membrane surrounding it that is easily disrupted by soap and water, and by many disinfectants. It appears to survive for days on a surface, at most, not for weeks like norovirus, the virus responsible for some stomach flus.
The most important rule: Clean first.
Clean kitchens at least twice a day.
The CDC suggests mixing 4 teaspoons of bleach per quart of water. Let it sit for one minute on the surface until you dry it off.
Be aware of the time a disinfectant needs to stay on a surface while air-drying. Sansoni notes that you should “read the product label on all disinfectants and wipes, because they have instructions on letting the surface stay wet or air dry for a certain amount of time, which varies by product.”
According to chemist William F. Carroll Jr. of Indiana University, “Cleaning removes dirt and the organisms that cling to dirt.”
Clean all commonly used surfaces: your kitchen counter, a table if you have an eat-in-kitchen, refrigerator door handles, cutting boards, stove knobs and cabinet doors. Make a checklist of places to clean and keep it handy — on a refrigerator door with a magnet, for instance. Simple soap and water will do. To clean your sponge at the end of the day, Carroll says to simply put it in the dishwasher with your dishes.
Wash your hands thoroughly.
Once you’ve finished cleaning surfaces, wash your hands thoroughly with soap and water for at least 20 seconds, following these CDC recommendations.
Remember not to wipe dirty hands on a clean towel, and make sure all the other family members do the same.
I WOULD ADD, especially in families whose members work in environments with several employees, that families NOT SHARE serving utensils at table.
That can be almost as bad as sharing a glass or cup.
One of the easiest ways to be infected by CV-19 is by contaminated hands.
We open a lot of doors, cabinets and drawers in a day, handle a lot of things at the stores, touch things like gas pumps, elevator buttons, telephones, copy machines, ATMs, mailbox lids/doors, the various buttons on our automobiles, or maybe we forget about things like keys, wallets and purses, that even the shoes we wear and take off once we're home can carry this virus.
People who wear eyeglasses that they may take off and lay on any surface, or adjust frequently throughout the day can pick up 'germs'.
That can be almost as bad as sharing a glass or cup.
One of the easiest ways to be infected by CV-19 is by contaminated hands.
We open a lot of doors, cabinets and drawers in a day, handle a lot of things at the stores, touch things like gas pumps, elevator buttons, telephones, copy machines, ATMs, mailbox lids/doors, the various buttons on our automobiles, or maybe we forget about things like keys, wallets and purses, that even the shoes we wear and take off once we're home can carry this virus.
People who wear eyeglasses that they may take off and lay on any surface, or adjust frequently throughout the day can pick up 'germs'.
As I've shown before, anyone coming home from work or from shopping or appointments may have come in contact with the virus.
It would be ideal if we all had a way to undress, shower and change into clean clothes BEFORE we reentered our homes, but that's just not possible.
"The virus that has devastated the world this year, SARS-CoV-2, is not a living organism. Viruses are not alive.
Think of them instead as biological machines, incredibly small ones.
Viruses have, in general, just two functions: they invade your cells, and then they borrow your own cells’ machinery to copy themselves.
Viruses have, in general, just two functions: they invade your cells, and then they borrow your own cells’ machinery to copy themselves.
(Note: for simplicity I’m describing viruses that infect humans, but in reality they infect pretty much every living thing, from bacteria to plants to animals.)
After making many copies, they break out, usually destroying the cell they’ve invaded, and do it again.
Here’s a weird thing about viruses. All living things on this planet are made from instructions encoded in DNA. Some viruses are also made of DNA, but many are made of RNA instead. RNA is a lot like DNA, but it doesn’t have that famous double-stranded helix structure; instead, it’s just a single strand.
Viruses cannot be seen under a normal microscope. Bacteria are huge compared to viruses; in fact, bacteria suffer viral infections just like humans do.
Viruses are also devastatingly effective at what they do (infecting living cells and hijacking those cells to make more viruses), which is why we will never rid ourselves of them.
While we can’t get rid of them, we can fight the viruses that cause human diseases, like Covid-19. The best way to do that is to prevent viruses from invading our cells.
How?
There’s only one good way that we know of so far, and that’s to use the human immune system to fight them off at the molecular level.
When a virus invades us, our immune system creates custom-designed cells that recognize and destroy the virus.
Here’s a weird thing about viruses. All living things on this planet are made from instructions encoded in DNA. Some viruses are also made of DNA, but many are made of RNA instead. RNA is a lot like DNA, but it doesn’t have that famous double-stranded helix structure; instead, it’s just a single strand.
Viruses cannot be seen under a normal microscope. Bacteria are huge compared to viruses; in fact, bacteria suffer viral infections just like humans do.
Viruses are also devastatingly effective at what they do (infecting living cells and hijacking those cells to make more viruses), which is why we will never rid ourselves of them.
While we can’t get rid of them, we can fight the viruses that cause human diseases, like Covid-19. The best way to do that is to prevent viruses from invading our cells.
How?
There’s only one good way that we know of so far, and that’s to use the human immune system to fight them off at the molecular level.
When a virus invades us, our immune system creates custom-designed cells that recognize and destroy the virus.
Then it becomes a race: if the immune system wins, it destroys all of the viral particles. If the virus overwhelms the host, the result can be fatal.
For Covid-19, most people mount an immune response quickly enough to avoid getting seriously ill. However, for those that don’t, the results are extremely serious."
For Covid-19, most people mount an immune response quickly enough to avoid getting seriously ill. However, for those that don’t, the results are extremely serious."
We must consider that there are "virus super-spreaders" among our population.
These are infected individuals who may not even know they have CV-19.
What is a superspreader?
The word is a generic term for an unusually contagious individual who’s been infected with disease. In the context of the coronavirus, scientists haven’t narrowed down how many infections someone needs to cause to qualify as a superspreader, but generally speaking it far exceeds the two to three individuals researchers initially estimated the average infected patient could infect.
What’s the impact of superspreaders for covid-19?
Researchers are beginning to come to a consensus after several new studies showing that coronavirus transmission more or less follows the 80/20 Pareto Principle (named after Italian economist Vilfredo Pareto): 80% of all consequences come from just 20% of the possible causes. For covid-19, this means 80% of new transmissions are caused by fewer than 20% of the carriers—the vast majority of people infect very few others or none at all, and it’s a select minority of individuals who are aggressively spreading the virus.
A person with COVID-19 may be contagious 48 to 72 hours before starting to experience symptoms. In fact, people without symptoms may be more likely to spread the illness, because they are unlikely to be isolating and may not adopt behaviors designed to prevent spread.
A study done by National Institute of Allergy and Infectious Diseases' Laboratory of Virology in the Division of Intramural Research in Hamilton, Montana used a nebulizer to blow coronaviruses into the air.
A person with COVID-19 may be contagious 48 to 72 hours before starting to experience symptoms. In fact, people without symptoms may be more likely to spread the illness, because they are unlikely to be isolating and may not adopt behaviors designed to prevent spread.
A study done by National Institute of Allergy and Infectious Diseases' Laboratory of Virology in the Division of Intramural Research in Hamilton, Montana used a nebulizer to blow coronaviruses into the air.
They found that infectious viruses could remain in the air for up to three hours. The results of the study were published in the New England Journal of Medicine on March 17, 2020.
What makes someone a superspreader?
We don’t yet know what it is about the biology of some people that causes them to be superspreaders. It might have something to do with increased viral loads and shedding more virus than is normal, but we still don’t know what would trigger this, let alone how to identify it through practical means.
What makes someone a superspreader?
We don’t yet know what it is about the biology of some people that causes them to be superspreaders. It might have something to do with increased viral loads and shedding more virus than is normal, but we still don’t know what would trigger this, let alone how to identify it through practical means.
ALL IT TAKES IS CLOSE CONTACT .
And remember, it's 18 feet, not 6 that this virus can travel with one cough, or sneeze.
VIRUS HOTSPOTS
These are areas that have higher than normal numbers of infected people.
Hotspots come and go and change from day-to-day.
Most states have a hotspot map you can refer to so you can avoid these areas when traveling.
NBC News has a daily updated map that shows the changes in each state, up and down, that you may find at least vaguely helpful.
As of today, Oct. 2, 2020, the states of Montana, Wyoming, Utah, Colorado, New Mexico and Wisconsin have all seen major increases in positive tests.
VIRUS HOTSPOTS
These are areas that have higher than normal numbers of infected people.
Hotspots come and go and change from day-to-day.
Most states have a hotspot map you can refer to so you can avoid these areas when traveling.
NBC News has a daily updated map that shows the changes in each state, up and down, that you may find at least vaguely helpful.
As of today, Oct. 2, 2020, the states of Montana, Wyoming, Utah, Colorado, New Mexico and Wisconsin have all seen major increases in positive tests.
Recently published research found that on average, the time from exposure to symptom onset (known as the incubation period) is about five to six days.
However, studies have shown that symptoms could appear as soon as three days after exposure to as long as 13 days later. These findings continue to support the CDC recommendation of self-quarantine and monitoring of symptoms for 14 days post exposure.
ALL of this taken together helps to explain why, even after taking every precaution, some will still contract CV-19.
The masks don't filter well enough, most people don't realize that new research has changed initial claims and created better protocols for staying just a bit safer, don't understand that enhancing one's immune system can help prevent or lessen the viral effect, or that something as simple as wiping down containers of foods that infected but maybe asymptomatic workers have handled can keep us a step ahead of this virus...hopefully.
Sometimes, just our biological makeup means we'll be more susceptible, no matter what we do and if we knew that, most likely we'd be far more cautious.
We don't have to become germophobic or adapt a dedicated hermit's lifestyle or become terrified to live normal lives.
But we also musn't be lulled by the mistaken idea that wearing a mask and social-distancing alone can keep us well.
Remember always that 98% of those who do contract CV-19 recover from it just fine.
Go ahead and get out when you can and enjoy beautiful Autumn.
The masks don't filter well enough, most people don't realize that new research has changed initial claims and created better protocols for staying just a bit safer, don't understand that enhancing one's immune system can help prevent or lessen the viral effect, or that something as simple as wiping down containers of foods that infected but maybe asymptomatic workers have handled can keep us a step ahead of this virus...hopefully.
Sometimes, just our biological makeup means we'll be more susceptible, no matter what we do and if we knew that, most likely we'd be far more cautious.
We don't have to become germophobic or adapt a dedicated hermit's lifestyle or become terrified to live normal lives.
But we also musn't be lulled by the mistaken idea that wearing a mask and social-distancing alone can keep us well.
Remember always that 98% of those who do contract CV-19 recover from it just fine.
Go ahead and get out when you can and enjoy beautiful Autumn.
Let the sun shine on you every chance you get.
I hope that each one reading here is and will be well.
___________________________
END NOTES:
A couple of fairly good resources for you:
-- Coronavirus Resource Center, Harvard's mostly sane advice and answers to common questions.
As coronavirus spreads, many questions and some answers
Updated: October 2, 2020
-- Enhancing Your Immune Response, also from Harvard Health.
OR, if you don't like Harvard, read <HERE>.
//WW




No comments:
Post a Comment